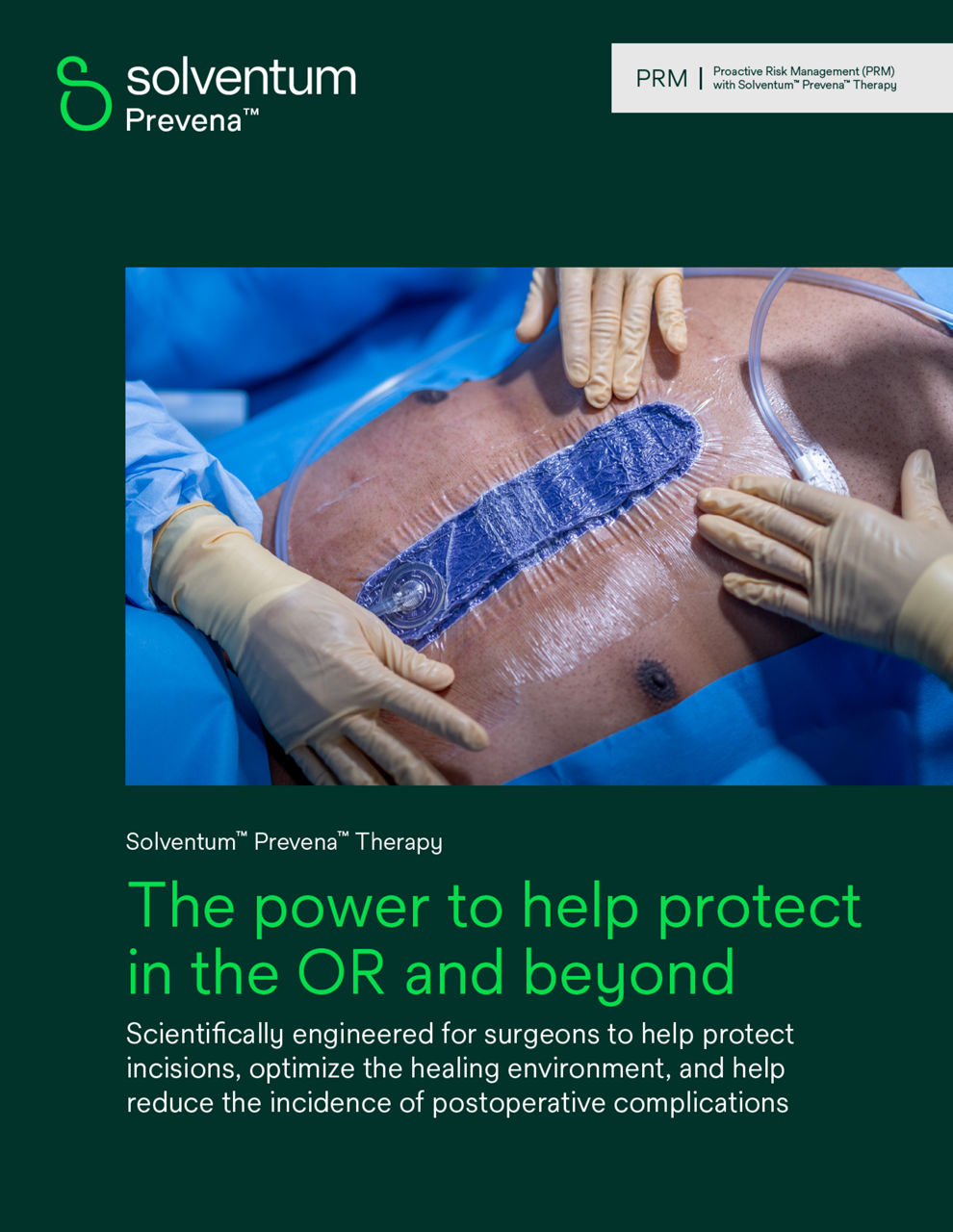
In today's healthcare landscape, where complex surgeries and patient comorbidities are prevalent, effective postoperative care is crucial to reduce extended hospital stays, readmissions and to improve overall patient outcomes. The Prevena Incision Management System is designed to proactively manage the environment of closed surgical incisions, such as superficial surgical site infections in Class I and Class II wounds* in patients at high risk for postoperative infections and incidence of seroma by maintaining a sealed environment with negative pressure therapy. This closed-incision negative pressure therapy (ciNPT) system provides:
- Protection: Prevena dressings create a barrier against external contamination
- Negative pressure: Delivers continuous -125mmHg negative pressure therapy for up to 7 or 14 days with dressing changes required at 7 days
- Incision support: Aids in keeping incision edges together, reducing lateral tension
- Fluid management: Removes fluids and infectious materials, helping to reduce edema
- Postoperative care: When used with legally marketed Prevena dressings for up to 7 days 3M™ Prevena™ 125 and 3M™ Prevena™ Plus 125 Therapy Units can help reduce the incidence of seromas and superficial surgical site infections (SSIs) in high-risk patients with Class I and II wounds
*The effectiveness of Prevena Therapy in reducing the incidence of SSIs and seroma in all surgical procedures and populations has not been demonstrated. Please see the full indications for use and limitations below.